Vanesa González Bellido, in addition to General Director of Fisiobronquial, is a professor in the Department of Respiratory Physiotherapy and Research at the Francisco de Vitoria University. The objective of the interview that we bring to Peques and Más is to explain the profession of respiratory physiotherapy in a simple, close and, above all, useful way for reading parents. Vanesa has provided an interview full of practical experiences with lots of information to know the discipline, its objectives and for whom it is especially recommended.
What is respiratory physiotherapy and why does it apply to children
Respiratory Physiotherapy is the most differentiated specialty of the whole of physiotherapy science. It acts on the respiratory system and specifically on the lung, which together with the heart and the brain are called points of the individual's trigone. Respiratory physiotherapy develops techniques for the prevention, cure and, where appropriate, stabilization of the alterations that affect the thoracopulmonary system. When you finish the degree you are a Physiotherapist, and like any other doctor who decides to study medicine and then has to specialize, I decided to study a specific field of Physiotherapy.
I think that knowing a field well, deepening it enriches you a lot, and is more responsible when facing your patients. For example, would a traumatologist be asked to operate at heart? That was what two great teachers taught me during the race. So when I finished, I took my bags, and I went to France, specifically to Paris, to study and work at Kinésithérapie Respiratoire (Respiratory Physiotherapy), one of the specialties that neither your own promotional partners wanted to study, nor in Spain had the recognition that I was looking for, and I knew I would find it there.
One of the fundamental objectives that the techniques of Respiratory Physiotherapy look for is the elimination of secretions, that is, to remove the mucus from the lungs and avoid bronchial obstruction. That is why it is so important in children, because a child's childhood revolves around his snot.
Bronchiolitis is the most common pediatric respiratory condition in children under two years of age, and determines edema, inflammation, hypersecretion in the bronchi and bronchospasm.
Due to the pathophysiology of the disease, the need for the respiratory physiotherapist is justified. If your child suffers from bronchiolits, it is because she has been infected by a virus called RSV (respiratory syncytial virus) although there are many more. These viruses generate symptoms such as fever, cough, pitos, shortness of breath, etc. in the child. The virus causes a series of damages in the bronchial tubes, including mucus plugs, bronchial closure, etc. That is what justifies our performance, what happens inside the child.
And in addition, babies have anatomical differences with respect to adults, which make them more vulnerable and with less response from the organism to these aggressions in the respiratory system.
It has been suggested that after the acute obstructive phase, RSV may persist latently in a low degree of replication in different lung areas avoiding complete elimination by the immune system and thus keeping it in constant stimulation. This would be responsible for chronic pulmonary inflammation, to act as a reservoir of infection, to cause reinfections and for changes in the pattern of said response observed in infants with RSV-induced bronchial hyperreactivity.
This could be summed up in the hundreds of times that parents ask us: are you always going to have mucus ?, and where does so much mucus come from ?, and these chest noises never stop ?, is it that it has become strained or is it that produces the same?
That is why the methodology that we apply in Physiobronchial for the elimination of bronchial secretions and to avoid that natural course of respiratory reinfections, becomes so important in a post-acute phase of bronchiolitis. Good management and control of bronchial secretions facilitates the deposition of the pharmacology prescribed by the doctor and helps the immune system to reshape the "normal architecture" that bronchus must have again as the child grows.
How respiratory physiotherapy helps children, especially in the treatment of bronchiolitis
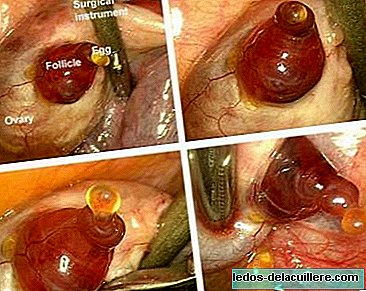
In this image you can see clearly so that parents understand what happens when a child suffers from bronchiolitis. The bronchial tubes close, become inflamed and produce a lot of mucus, and that happens in a matter of hours.

The child may go through an acute phase even requiring hospitalization for 3 to 7 days in need of oxygen, and medications that are administered in the form of aerosols. There are children who do not need hospitalization in that first bronchiolitis because clinical severity does not require it and is determined by their doctor. In both cases, in the case of bronchiolitis, a medication is prescribed that parents know as puffs or aerosols and begin to notice what the bronchiolitis bug does: cough, chest noise and fatigue.
What will Respiratory Physiotherapy do for them ?, attack those symptoms, how ?, removing all the mucus that has invaded that bronchus, helping it to breathe better and something very important, allows the medication to take effect. And it is that a medication such as ventolin, salbutamol, budesonide, etc. What they are trying to do is open the bronchus and if you encounter all that mucus, you will not be able. The physiotherapist must know what lies ahead, in which phase is that medically diagnosed bronchiolitis and decide on the basis of a physiotherapeutic assessment what to do at each moment.
What is the physiotherapist's responsibility?
I have a center where only respiratory conditions are treated and many parents ask us about other issues, colic, congenital torticollis, neurological therapies, etc. My answer and that of my team is clear: we only attend respiratory. Because we lack training in other fields, at the level of demand and quality that we demand in the respiratory system.
There are doctors who think that Respiratory Physiotherapy in case of bronchiolitis should be contraindicated, there are many fellow physiotherapists or parents who tell me, how is that possible ?, because it really is true. That is, one must know when to act in case of bronchiolitis, how to assess it, know the medication that is being taken, and if it has more processes associated with that bronchiolitis why it can modify your way of acting.
For example, a ten month old baby who suffers from bronchiolitis. When he arrives at my center, the first thing is to know his medical diagnosis, to know if he is already in a post-acute phase, through a clinical interview with the parents, and an assessment of the baby through auscultation, clinical observation and pulse oximeter. Imagine that during the session the baby expels secretions that attract our attention because we see them, smell and touch them, plus the symptoms and signs we have asked the parents, do not sleep well, do not satiate when they eat, etc. REFLUX! This baby has a possible reflux that can be a cause or consequence of bronchiolitis, that is not my job, my job has been to suspect that this child may have a reflux, that I must modify my manual techniques when it comes to attending to him, and know when I have to put the next review.
It is very important to see many patients with the same symptoms. If at the end of the day you only attend to this type of patient, you know very well that the frequency makes you get these suspicions that are so successful for the baby's health and for your treatment. Many doctors tell me the same thing that children send us and that they always tell parents: you see there they know what they do!
By the way, I know that many parents think that these are a bit "aggressive" therapies and I always answer the same thing: we would never do anything that would harm a child because that is not allowed. What I know that impresses parents or doctors who visit us at the clinic is the amount of mucus that a four-month-old, two-year-old or ten-year-old child can expel by mouth. The fact that during the session we quantify, touch, observe the mucus color, it is a successful indication of the session. Many parents who come from other centers tell us this kind of thing, my mother, this is mucus, they didn't get anything out of there!
Every year we try to present at the Annual Congress that celebrates the Society of Pediatric Pulmonology (SENP) some communication so that our work is known. We do not attend because yes, at all, we attend with a scientific base and protocols that we evidence day by day with our results. For example, we have conducted a study on gastroesophageal reflux in recurrent wheezing during a session of Respiratory Physiotherapy. We also present others about bronchiectasis. If parents want to read them and are interested, it is possible to review them on our website.
In which countries physiotherapy is applied to children
Respiratory Physiotherapy is applied in many countries of the European Union, such as France, England, Belgium, etc. When I decided to work at the Necker Hospital in Paris, I did it because I was already influenced by the Francophone school in front of the Anglo-Saxon. That is, he preferred to deepen techniques and procedures with a more current and more scientific basis, than the one that was being practiced at the Brompton Hospital (London), obsolete techniques such as postural drainage or claping. Curiously, claping or “tapping the back” is an indication that many pediatricians give to moms when the child has snot, and respiratory physiotherapists always tell them that they should not be tapped because it can be harmful to the child.
My team and I have acquired deep slow inspiration techniques and acceleration of expiratory flow as bronchial hygiene maneuvers from Francophone heritage. I maintain a close training relationship with kinesiologists from Chile and Argentina, two countries where there is a recognition of respiratory kinesiology. When I was at the Roberto del Rio Hospital in Santiago, Chile, what caught my attention was not so much the action protocols that you also learn, but the "professional role" that respiratory kinesiologists have there.
For example, in Chile it is like in France, there is a physiotherapist who depends on the Service where he serves. In Chile the first time I went coincided with the influenza A epidemic, and I remember that there were physiotherapists even in the ER! and the same happened in the Health Centers. That is, there were physiotherapists in all the places placed. That is important, to become necessary for doctors, for families, for all those who work for the child's health care.
What kind of children go to the Respiratory Physiotherapy consultation
Children with two types of conditions come to my office: those that affect extrathoracic pathways, for example, recurrent otitis and those that affect intrathoracic pathways (lungs, bronchi), for example, bronchiolitis or pneumonia.
The most frequent, are those that affect the lung, but this year we have received many children for recurrent otitis with great success not only with respiratory physiotherapy, but also with the referrals we make of these children to physicians who give our confidence that They find the problem. The "vegetations" child is the typical child who always has green mucus in his nose, snores at night, his mouth smells a lot and sometimes has a special palate shape. All this together with the boogers that we take out, we immediately tell parents that we must coordinate with the ENT to establish an effective treatment, and prevent those ears from suffering in the long term.
Bronchiolitis is the most frequent pediatric respiratory condition, a syndrome that affects 70 to 80% of cases in children under two years, with a peak frequency between 2 and 10 months.
The incidence throughout the first years of life is 20 to 25 per 100 children and per year. These conditions have a great impact on the quality of life of patients and family members (absenteeism at school, work leave, work leave, etc.), and a significant increase in the use of health resources (Emergency, Hospitalization, medications , etc).
Bronchiolitis is a disease that evolves from seasonal epidemics of a winter nature, observed in the northern hemisphere, especially between December and March. Most of the time it starts with an extrathoracic airway condition and, after 48 to 72 hours, it extends into the intrathoracic airways. After the first episode of bronchiolitis, 50% of children will have at least one other episode and 30% of children hospitalized for acute bronchiolitis will have recurrences in the years following infection. This means that in recent years the relationship between acute bronchiolitis induced by viruses, mainly respiratory syncytial virus, and the subsequent development of bronchial hyperresponsiveness and infant asthma have been studied.
The episodic wheezing they occur during discrete periods of time that often coincide with viral colds, but outside of them there are no wheezing. On the other hand, in wheezing caused by multiple triggers, although viruses remain the main trigger in these preschoolers, other agents such as exercise, tobacco, allergens, etc. may be involved.
The pattern that is most repeated is that of children with transient early wheezing that would be episodic wheezing. These occupy 60% of my patients. They appear in the first year of age and normalize before 3-5 years. They usually have no family history of asthma or allergic sensitization. But other variables such as prematurity, male sex, contact with siblings and other children in daycare, smoking during pregnancy and postnatal exposure to tobacco smoke may be associated. A correct diagnosis and treatment in these children and does not have to damage the lungs in the future when they are older.
And then there would be the children with non-atopic wheezing They occupy 20% of my patients, where the picture begins before the year of age and the episodes last beyond 3-5 years. The beginning of the clinic is related to viral infections such as rhinovirus (RV) or RSV.
There is also the group of children with persistent atopic wheezing They manifest themselves from the first year of age and have a personal history of atopy, atopic dermatitis, food and environmental allergies, and a family history in the first degree of asthma. In this group we have 15-16 year old kids with asthma that curiously it is they who tell their parents: "Dad calls the consultation I need my physio". They are phenomenal after a session and know that all the guidelines we give them are useful. And that is what a boy of that age is looking for.
The diagnosis of asthma in infants and preschoolers continues to present difficulties, in 1998 the III International Pediatric Consensus defines “infant asthma” as that situation in which three or more episodes of wheezing and / or cough occur, in a clinical setting in the diagnosis of asthma is the most likely and after having excluded other less frequent processes. This conceptually strategic definition maintains its relevance (PRACTICALL consensus, 2008), since it includes the expression of the disease (wheezing, cough), the recurrence of the episodes (three or more) and the absence of other pathologies (wheezing and coughing they are not equal to asthma).
Currently we do not have sensitive and specific markers or biological causes that allow us to distinguish infants with recurrent wheezing that are going to be future atopic asthmatics and that are also those that having been born with a normal lung function will present an irreversible deterioration of the same in the first Five years of life. They are also the ones that will present the greatest persistence and severity of the disease, as well as the greatest number of relapses. To identify this group of infants, Castro-Rodriguez et al. proposed the predictive index of asthma (IPA).
Children who have frequent recurrent wheezing below three years of age and meet at least one major criterion or two of the three minors will have a high probability of suffering a persistent atopic asthma in the future, that is, in the Predictive Index of Asthma (IPA). This is somewhat complex, if parents have doubts that they write to me that I kindly explain it to them.
And then in addition to this whole group of “bronchiolytic, asthmatic”, we have children with chronic diseases such as bronchiectasis, cystic fibrosis, primary ciliary dyskinesia, cardipatias, etc.
And we also treat neurological patients who teach us so much humanly speaking. About these chronic patients we have published a lot in the last three years. Many of these publications can be accessed on the Fisiobronquial website.
How respiratory physiotherapy is complemented with the pharmacological treatments prescribed by doctors
Physiotherapists must perfectly master pharmacology because it is an integral part of their therapeutic arsenal. Physiotherapists do not prescribe prescriptions, but we must know the effect, the form of administration, etc. of the drugs that doctors prescribe to our children, and even recommend doctors to use any of them.
I give you examples: I receive children from all over the Community of Madrid, and sometimes even from outside Madrid. The fact of seeing so many children from so many areas, gives us a very rich clinical perspective, and we see the differences in treatment that sometimes occur when facing the same pathology. If we take care of a child because of his medical history, because of the secretions we take out, because of the continuity of the symptoms he presents, etc. and we believe that you have to take a complementary pharmacological treatment, we send a report to your pediatrician in medical terms so that we speak the same language that justifies that recommendation very well. For example, recommend budesonide every 12 hours for at least 6 weeks. In this way, as the child has the cleanest bronchi now with respiratory physiotherapy, the drug particles will deposit in the bronchus and optimize its effect.
Sometimes, before a session of respiratory physiotherapy, you need to apply an aerosol such as Ventolin to open the bronchi better and there is less difficulty in expelling the mucus. The physiotherapist should know how to administer the drug, and when is the best time. Mucolytics such as mucosan, fluidase, flumil, etc. They are not advisable to treat the accumulation of bronchial secretions in the child. Its character is sometimes irritating and can prolong the cough, and this in turn, keep hypersecretion. I always tell parents that there is no drug that expels mucus.
What is the return on investment in a physiotherapy treatment
The price of the session in my consultation is 37 euros. The average number of sessions that children receive in my consultation is 6-7 sessions, one session per month, more or less, every 25 days. The total would be 250 euros, which if you distribute it a month is to dedicate every month 37 euros in the health of your child.
Children should come every 25-28 days, and thus prevent them from falling ill. Should physiotherapy be done if the child is well? Most of the children we have talked about previously suffer from bronchiolitis and become small asthmatics who will have good and bad days. With the virus they get worse, which is what usually happens from November to April and more if they go to daycare centers. These children take a background medication, such as budesonide or singulair, which in their case serves to prevent the mucus from accumulating.
In these cases, we recommend that you come every month especially winter. Even so, I insist, it is not money 250 euros if we count what is an income for these children, the absence to the nursery and the work leave of the parents.
On the other hand, a child who only suffers from high-altitude colds, is not to have to come every month, but if the parents at the first symptoms it is better to bring him to prevent the mucus from going down to the chest and causing damage greater. To me, it was one of the things that caught my attention in France, parents have this habit of going down to the Physiotherapist's cabinet as soon as they have colds or runny nose, and avoid medications.
Look, my team and I are preparing a publication now on The recurring Sibiltante in which the number of crises suffered by these children during seven months of a year, the visits to the ER and school absenteeism during that time are mentioned . We have observed that children who regularly attended Respiratory Physiotherapy, school absenteeism in Infant Schools is much smaller, and that is very important today.
There are many who need to leave children in school because they do not give them days off at work, it is essential to invest in children's health day by day, month by month, because in the long run it is not money. That is what we wanted to capture in this study, in addition to demonstrating that children suffer less crisis, which means less medication and fewer visits to the ER.
How old are the children who come to the consultation
We have children of all ages, from 15 days of birth to 18 years. The fact of attending so many pediatric patients and covering so much age range, allows us to know what each patient needs based on their pathology, age, collaboration and state in which the patient comes.
70% of the children who come to my center are under 3 years old, the other 30% would correspond to children between 4 and 18 years.
The maneuvers are modified according to the patient's age due to physiological and anatomical issues. In addition, as children are older than four years of age, we use instrumental aids that make treatment more effective.
The growing incidence of childhood respiratory diseases, we mentioned earlier, is linked on the one hand to the evolution of the germs responsible for respiratory infections and the current prevalence of viral infections over bacterial infections, and on the other hand to a set of environmental factors in which air pollution and life type are associated.
One of the pathologies that we most like to solve are atelectasis or pneumonia, because it is very gratifying to see on the plaque that parents bring as the mucus plug that collapses / occupies an area of the lung is observed, and in an average of five sessions We solve it. When they make the control board it looks perfectly like that “little spot” is no longer visible, but do not think we get rid of the child we always try to receive in the following months (more or less 3-5 months after that frame) Some follow up session.

In the picture you can see the case is of a seven-year-old boy who had suffered several cases of pneumonia. That mucus accumulated and formed plugs until they reached pneumonia. The boy arrived at my center on July 23, just out of a Hospital in Madrid, he was referred to me by a pulmonologist. The plate on the right of day 23 reveals a mucous plug (white area) in the middle of the right lung. On the left plate, after five days of treatment, the pneumonia is resolved and the area is well ventilated (black zone). The child runs, jumps, does not have a cough and the most important prepared to attend his school and not miss this year to class.
Where can we find Fisiobronchial.
When I arrived from France 11 years ago, I was very clear that I wanted to set up the same center model as where I worked in the evenings in Paris (in the morning I worked at the Hospital). I knew that I was facing something very hard here in Spain for a person who starts and that is the ignorance of what one does. I worked very hard, training, dissemination, in short, everything was coming slowly until now.
Two years ago Fisiobronquial was recognized as the only center of Respiratory Physiotherapy of the Community of Madrid that obtained the certification by AENOR, in the diagnosis and physiotherapeutic treatment of pathologies of the respiratory system.
For me, it was not a simple seal of quality, it was the recognition of all my years of work, it was like saying now if I can say “That those of Coslada are the pioneers” in this field. Many fellow physiotherapists put their hands to my head when I tell them that I only attend respiratory, because they always tell me "but you live from it!". Yes, I answer, it is more this year we have begun to collaborate with another center in Madrid capital and it has been a success.
All my team is made up of me, what's more, they have all been my students at the University where I teach classes with which I know them since they began their studies, until they finished them and they all had to be clear that they had to specialize in an area because In my center we do not see other patients except respiratory. To all of them I owe them very much, and more in the last two years where we have set very high goals in the subject of research and publications, and we are getting very nice things from the Fisiobronquial center.
Another aspect that I would like to highlight for parents who read to us is very important that they know that the Respiratory Physiotherapy Centers must also be equipped with apparatus for therapies. Because we must offer results and scientific evidence to our patients. In my centers, I have all kinds of devices that may not sound like names to parents but I like to say it because it was many points in my favor for AENOR to certify this center as a center of Physiotherapy in diagnosis and physiotherapeutic treatment of pathologies of the respiratory system. This happens a lot with the chronically ill that when they come the first time and see everything we do to them, we put and send them to do at home because they are surprised at the differences with other centers.
On the Internet page of Fisiobronquial I dump a lot of information every month, from very simple articles and presentations for parents, to reports in the press or television. To make an appointment you can use the phones 916741270 or 695130011 or use the email: [email protected]. We always tell you that any questions call us, consult us and of course ask your pediatricians that many know us.
I am aware that the images that I have posted on the web, or the last video that we have been made on Spanish Television is sometimes a bit “strong”, but I like to hang the truth and reality, without hiding anything because I have nothing What to hide
Y So far the interview with Vanesa González Bullido, expert in respiratory physiotherapy. We thank you for the amount of data and experiences you have provided us and we hope that readers find it useful and appropriate to consult, contrast and facilitate decision making. For parents who come to this article from a search engine can be especially useful and practical information.